Flesh Eating Bacteria is an Initial Misnomer
Read this Article on my Website
There has been a significant up tick in the number of news outlets reporting "flesh eating bacteria" commonly known as Vibrio Vulnificus. In Latin, the term vulnificus means "wounding". Specific strains of this gram-negative bacteria include Vibrio parahaemolyticus, Vibrio vulnificus, Vibrio alginolyticus and about nine others that can cause an infrequent infection called vibriosis. V. vulnificus is the most pathogenic of the Vibrio genus: wound infection mortality rates are as high as 18% and fatalities have occurred as soon as 48 h following exposure. Infections are highest between April and October. Overall annual costs associated with this pathogen are estimated at US$ 320 million, making it the most expensive marine pathogen in the USA to treat.
This bacteria does not actually "eat through your skin" but instead needs a breakdown in the skin, such as a cut, bad burn, piercing and even tatoos, which allows it to begin a process called necrotizing fasciitis.
This is when, in about 10% of cases, the actual "flesh eating" occurs via enzymes called proteases. While media reports say the Vibrio bacteria causes this problem, Group A Streptococcus causes it more often (48%).
Thriving Locations
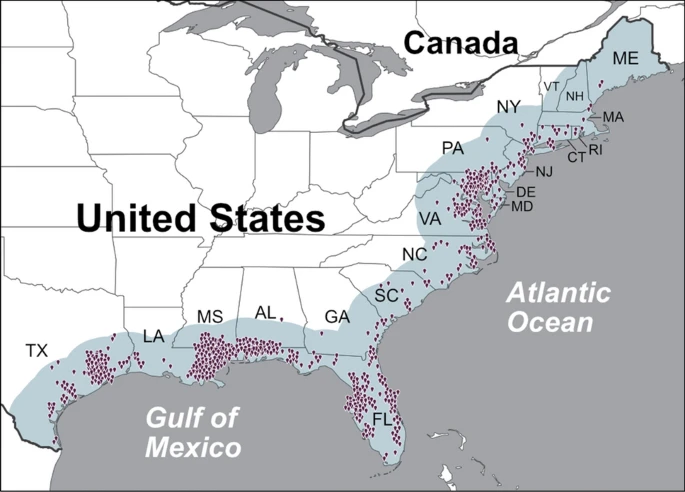
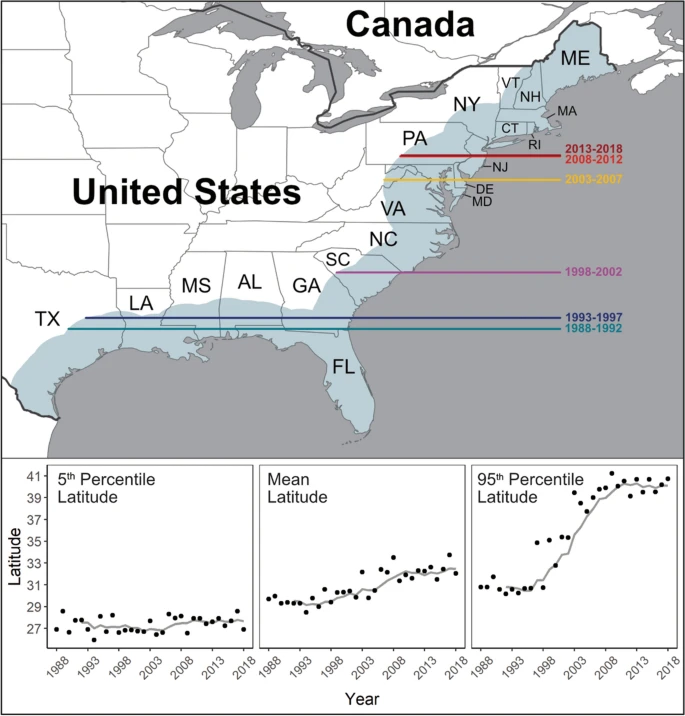
V. vulnificus thrives in warm, mixed salt and fresh or brackish waters and is most abundant in shellfish during warmer months. Its range is expanding northward, with cases increasing eightfold in the Eastern USA over the past 30 years. Climate change is expected to further increase both the incidence and geographic spread of infections. These associations with climate have led to Vibrio species being collectively recognised as a “microbial barometer of climate change.
Historical distribution of V. vulnificus infections between 2007 and 2018.
Latitudinal Change over Time
Signs and Symptoms of an Infection
Onset of symptoms usually occur within 24 hours. An early sign is redness and swelling that occurs within hours. You may also see bruising-like-discoloration, as seen in the picture below, along with significant pain, swelling, warmth, fever, blistering bullae, high heart rate, and clear or pus-like discharge. Underlying gas can be seen on X-ray.

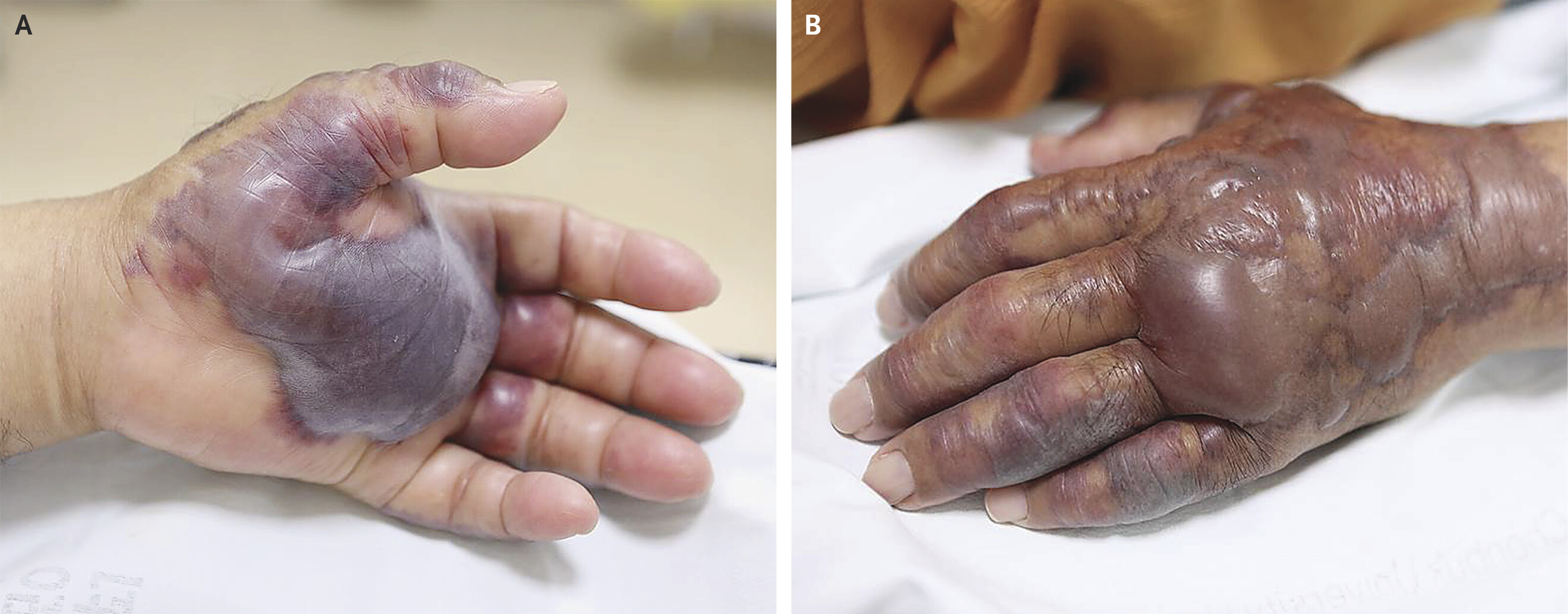
Image Credit: July 25, 2018 | N Engl J Med 2018;379:375 | VOL. 379 NO. 4
Steps to Prevent Infection
If you have an open wound, stay out of saltwater or brackish water, if possible. This includes wading at the beach. Cover your wound with a waterproof bandage if it could come into contact with coastal waters or raw seafood, its drippings, or its juices. This contact can happen during everyday activities, such as swimming, fishing, walking on the beach, or even shucking oysters. It also could happen when a hurricane or storm surge causes flooding. Immediately wash wounds and cuts thoroughly with soap and clean running water after contact. If you are at increased risk for infection, wear clothes and shoes that protect you from cuts and scrapes when in coastal waters.
Treatment and Prognosis
Do not delay seeking help. Time to treatment and fatality rate are directly proportional. Immediate surgical intervention (fasciotomy or debridement) within 12–24 hours of admission significantly reduces mortality; delays beyond 24–72 hours are linked to worse outcomes. Wound cultures and blood cultures, positive in approximately 30% of patients with septicemia due to v. vulnificus wound infections. Often times multiple surgeries are requied increasing the length of stay in the hospital. Unfortunately some cases lead to amputation.
Empiric antibiotics should cover Vibrio species (e.g., doxycycline plus cephalosporins or quinolones) and, due to rising antibiotic resistance, be adjusted based on sensitivity. Even with antibiotics surgery is still required for debridement which prevents contiguous spread and bacterial seeding.
Mortality rates increase with delayed treatment, shock, or underlying comorbidities such as diabetes, chronic kidney failure, and/or decompensated liver disease like alcoholic cirrhosis and hepatitis c. Hyperbaric oxygen (HBO) therapy and vacuum assisted closure (VAC) therapy can be administered in stable NF patients for improving wound healing.
A Quick Note on The Disruption of the CDC
With the interruption of CDC policies and loss of several key personal it will become increasingly difficult to know where outbreaks of near-fatal infections occur. I encourage everyone with cases of rare infections like the one in this publication to share them on social media and/or with your local health department. This will help spread the word and alert others.
Conclusion
Vibrio vulnificus skin infections while infrequent are notable for their rapid progression from redness and swelling to blistering, severe pain, and potentially tissue death. Early recognition and urgent medical attention are critical to prevent severe complications. As always, alert your doctor if you have concerns.
Checkout the latest Clear Health Podcast episode with Dr. Lorena Pacheco PhD from Harvard as she discusses the power of an Avocado!
References
- Kuo, Y., Shieh, S., Chiu, H., & Lee, J. (2007). Necrotizing fasciitis caused by Vibrio vulnificus: epidemiology, clinical findings, treatment and prevention. European Journal of Clinical Microbiology & Infectious Diseases, 26, 785-792. https://doi.org/10.1007/s10096-007-0358-5.
- Archer, E., Baker-Austin, C., Osborn, T., Jones, N., Martínez-Urtaza, J., Trinanes, J., Oliver, J., González, F., & Lake, I. (2023). Climate warming and increasing Vibrio vulnificus infections in North America. Scientific Reports, 13. https://doi.org/10.1038/s41598-023-28247-2.
- Coerdt, K., & Khachemoune, A. (2021). Vibrio vulnificus: Review of Mild to Life-threatening Skin Infections.. Cutis, 107 2, E12-E17 . https://doi.org/10.12788/cutis.0183.
- https://www.cdc.gov/vibrio/about/index.html
- https://www.cdc.gov/vibrio/hcp/clinical-overview/index.html




